Understanding Allergy-Induced Cough
Ugh, that cough. The one that just won’t go away. If you’ve dealt with an allergy-induced cough, you know exactly what I’m talking about. It’s not just a little tickle; it’s this annoying, persistent thing that can honestly ruin your whole day. It all starts when your body just kind of freaks out over something totally normal, like pollen or the cat deciding your face is a great place to nap. Your immune system goes into overdrive, your airways get all inflamed, and boom—you’re coughing.
I used to think a cough was just a cough, but this is different. It can be a dry hack or a gunky, mucus-filled nightmare, and it seems to get so much worse at certain times of the year or, you know, whenever I decide to dust the shelves. And if you’ve already got something like asthma going on, it can feel ten times more intense. It took me a while to figure out the triggers and what was actually happening. I also read somewhere that things like being around smoke can make it even worse, which makes total sense. It’s like, your airways are already irritated, so that just adds fuel to the fire. So yeah, figuring all this stuff out is the first step, I guess.
Causes of Allergy-Induced Cough
So what’s actually causing all this misery? It's usually the stuff we breathe in without even thinking about it. Here’s a quick list of the usual suspects:
-
Pollen from trees, grasses, and weeds
-
Dust mites found in bedding and upholstered furniture
-
Pet dander from dogs, cats, and other furry animals
-
Mold spores present in damp indoor spaces
And sometimes, it’s not even what you’re breathing. I’ve heard that food allergies can sort of indirectly cause a cough by leading to postnasal drip, which is just as gross as it sounds. Getting an allergy test can be a real eye-opener. It really helps to know exactly what you’re fighting. Plus, the seasons totally play a part. Spring is pollen-pocalypse for so many people, and then in the fall, when it’s all damp, mold can pop up. It’s like there’s always something.
Symptoms and Diagnosis of Allergy-Induced Cough
The cough is usually the main event, but it often brings along a bunch of other unwelcome friends. This is what it usually looks like for us:
-
Nasal congestion and runny nose
-
Sneezing and itchy eyes
-
Shortness of breath or wheezing
-
Postnasal drip
Getting a diagnosis usually just means a trip to the doctor. They’ll take a look, ask a bunch of questions about your history, and maybe suggest an allergy test—either a skin prick or a blood test. Once you know what’s causing it, you can actually make a plan. Sometimes the doctor might have you try an antihistamine for a bit just to see if it helps, which is a pretty good clue right there. I’ve found that keeping a little diary of symptoms is super helpful. Just jotting down when the cough gets bad can help you connect the dots to what you were doing or where you were that day.
Over-the-Counter Treatments
Alright, so when that cough hits, the first place I usually turn is the pharmacy aisle. The over-the-counter stuff can be a real lifesaver for just getting through the day, even if it’s not a permanent fix.
Antihistamines for Allergy-Induced Cough
Antihistamines are pretty much my first line of defense. They work by blocking this thing called histamine, which is the chemical your body releases when it’s having an allergic reaction. It’s the stuff that makes you cough and sneeze and itch.
You’ve probably seen brands with loratadine or cetirizine on the box; those are the ones that are supposed to be non-drowsy. And they mostly are, but I’ve learned that everyone reacts differently. The older ones, like diphenhydramine, will knock me right out. It’s really a trial-and-error thing to find what works for you without turning you into a zombie. I also feel like taking it before I know I’m going to be around a trigger—like before visiting a friend with a dog—works way better than waiting until I’m already a mess.
Decongestants and Their Effectiveness
If postnasal drip is the problem, decongestants can really help. They clear up that stuffy feeling in your nose, which can stop the drip that’s making you cough. But, and this is a big but, you have to be careful with them. I found out the hard way that ingredients like pseudoephedrine can make your blood pressure go up, so they’re not for everyone, especially if you have heart issues.
You’re also not supposed to use them for more than a few days. If you do, you can get this thing called rebound congestion, where you end up even stuffier than when you started. It’s so frustrating. If you’re not sure, it’s definitely worth asking a doctor. For a gentler option, I’ve found that a simple saline nasal spray can do wonders just by keeping everything moisturized, without any of the side effects.
Prescription Treatments
Sometimes, the over-the-counter stuff just doesn’t cut it. When the cough is really bad or just won’t quit, it might be time for something stronger from the doctor. These are the big guns that can really get the inflammation under control.
Steroid Medications for Severe Cases
When things are really inflamed, a doctor might prescribe corticosteroids. These are serious business for calming down your whole respiratory system. You’ve probably heard of nasal sprays like fluticasone; that’s a common one they use.
They work, they really do, but it’s something you have to be on top of. If you’re using them for a long time, the doctor will want to keep an eye on you for side effects. And you can’t just stop taking them cold turkey, or your symptoms can come roaring back. It’s one of those things where you have to follow the instructions exactly.
Leukotriene Modifiers and Their Role
This is another class of prescription meds I learned about. They’re called leukotriene modifiers—montelukast is a common one. Basically, they block other chemicals in your body that cause allergic reactions and inflammation.
They seem to be especially helpful if you’re dealing with both allergies and asthma. It’s something you’d need to check in with your doctor about regularly, just to make sure it’s working and not causing any issues. But I’ve heard from people that these can be a total game-changer, helping them feel so much better and get back to their normal lives. It’s not a magic pill, though. It’s part of a bigger plan that should still include trying to avoid your triggers.
Natural Remedies and Lifestyle Changes
Okay, so beyond the pharmacy, there’s a lot of stuff you can do at home that actually helps. For me, pairing medical treatments with some more natural approaches has made a huge difference.
Dietary Adjustments for Allergy Relief
I’ve been learning so much about how food can affect allergies. It seems like eating anti-inflammatory foods—things like fish with omega-3s, lots of fruits and veggies—can help your body calm down a bit. I mean, a healthy diet is good for everything, right? So it makes sense it would help your body not overreact to allergens.
On the flip side, I’ve noticed some foods can make things worse. For some people, it’s dairy; for others, it’s processed stuff. I started keeping a food diary for a while, and it was really interesting to see if I could connect a bad cough day to something I ate. It’s worth a try. Loading up on things like berries and spinach, which are full of antioxidants, can’t hurt either.
The Impact of Exercise and Hydration
Getting some regular exercise is another big one. It just seems to help keep my lungs strong and my body feeling more resilient. I try to be smart about it, like going for a bike ride instead of a run through a grassy field when pollen is high.
And hydration—this is so, so important. Drinking a ton of water helps thin out all that mucus, which makes it way easier to get rid of. It’s such a simple thing, but it provides real relief. Sometimes a warm herbal tea, like peppermint or ginger, feels really soothing on my throat, too. Oh, and a humidifier in the bedroom at night? A total game-changer for easier breathing.
Preventive Measures for Allergy-Induced Cough
While having treatments on hand is great, not having the cough in the first place is even better. Prevention is all about figuring out your triggers and then trying your best to stay away from them.
Allergen Avoidance and Control
This is my checklist for keeping the house from becoming an allergy trigger zone:
-
Using air purifiers with HEPA filters to snatch allergens out of the air.
-
Regularly washing bedding in hot water to kill off those lovely dust mites.
-
Keeping windows closed during peak pollen season (as much as it pains me to shut out the fresh air).
-
Trying to avoid being outside for too long when the pollen count is through the roof.
Creating an allergy-proof home, or at least a less-allergenic one, has honestly made such a difference. It feels like having a safe space to retreat to when the air outside is trying to kill you.
Regular Health Check-ups and Allergy Tests
Staying in touch with your doctor is key. They can help you see if things are getting worse and make adjustments to your plan. And getting allergy testing done was a turning point for us. It felt like we finally had a real roadmap instead of just guessing.
This kind of proactive approach means you can tweak your lifestyle or medications as needed. It’s all about staying ahead of it. Keeping that symptom diary I mentioned earlier is really useful for these appointments, too. It gives the doctor real information to work with, which can lead to better, more effective strategies.
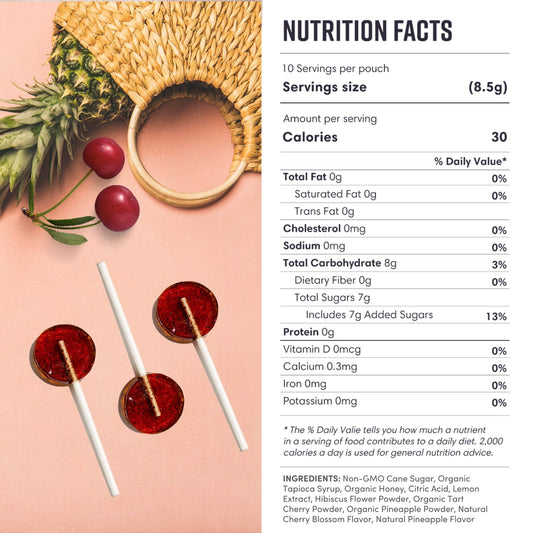
Trying to manage a cough from allergies can feel like a full-time job, but once you find the right combination of things that work for you, it really is manageable. Something as simple as our MommaBear Organics Lollipops can be a really nice, natural way to help soothe some of those symptoms. By figuring out your triggers and working with a doctor, you really can find relief and get back to enjoying your life.
It's a journey, for sure. Some days are better than others, and I’m still learning what works best for our family. It’s all just trial and error, isn’t it? Just trying to do the best we can.